Is your baby or toddler waking really frequently at night?
Maybe they’re waking hourly or every sleep cycle (or even more often!) for some or all of the night…and you’re wondering what on earth’s going on?
Frequent night wakings are not only EXHAUSTING, they can be a real puzzle!
But now you’re here, hopefully I can help shed some light on this for you.
But before we get into the likely culprits, please know that…
Firstly: you’re not alone
Very frequent night waking is a common baby sleep challenge – in fact it’s probably the most common baby sleep ‘problem’ that I help parents with.
Secondly: there is good news!
Once you know what’s causing your little one’s wakefulness, it’s usually possible (with a few tweaks / changes) to get to a place where they’re sleeping for longer stretches – and everyone can have more restful nights! Zero sleep training required. This is what I help parents with every day in my 5 Day Baby Sleep Mini-Course, and my flagship program: Baby Sleep Revolution™.
Okay, so let’s get into it and take a look at…
Common Causes Of Frequent Night Waking
1) Temporary illnesses
Many parents find that their little one more wakeful when they’re unwell. And that’s simply because many illnesses cause pain or discomfort which can make it hard for little ones to sleep soundly. And if your little one is breastfed, they may also want to feed more frequently at night for comfort/pain relief and to dose up on antibodies too.
So if your baby or toddler suddenly becomes more wakeful, definitely keep an eye out for signs of illness – sometimes it can take a day or two for symptoms to become visible to parents or caregivers.
The good news is that sleep usually improves again once a little one is feeling better – so if this is the cause of the wakefulness, hopefully it won’t be for too long,
2) Health conditions
While they only affect a relatively small percentage of babies and toddlers, it’s really important to be aware that there are a number of health conditions that can affect sleep and cause a little one to be more wakeful than they otherwise would be.
Health conditions can disrupt sleep either because they cause pain or discomfort, or because they interrupt systems in the body or brain.
Some of the more common health conditions that have been found to be associated with increased wakefulness include: food allergies [1], atopic dermatitis (eczema) [2], feeding issues that can prevent baby from feeding to full satiation [3], sleep disordered breathing (including sleep apnea), iron deficiency anemia (IDA) [4], gastroesophageal reflux disease (GERD) [5] and some neurodiverse conditions [7], [8], [9].
Please note these are examples and not an exhaustive list of potential possibilities. If you have any concerns about your little one’s health or development, it’s important to investigate with a qualified healthcare professional.
If you don’t have any specific concerns about health or development, it may still be worth having a review with your healthcare provider, even if just to rule them out for peace of mind.
3) Separation stress (Separation anxiety)
I’m not a huge fan of the term ‘separation anxiety’ because it’s actually 100% normal for babies to need to sleep close to their parent or caregiver, AND 100% normal for them to become stressed if that need is not met.
It’s the biological norm for human babies to sleep in close proximity to a caregiver – either in their own little bed within arms reach, or bed sharing (sharing the same sleep surface) with their parent/caregiver. They’re wired to sleep this way for safety, warmth and to be able to feed on demand.
It’s really only been in the last century or two – and mostly in Western (especially English-speaking) cultures – where it has become more common for babies and children to sleep separately from their parents/caregiver, often in their own nursery / bedroom.
Some babies and toddlers are okay with this kind of separation at night time (side note: from a safe sleep perspective, sleeping in a separate room isn’t recommended until at least 6 months or older).
But some have a strong need for closeness at night and can become stressed if they can’t sense their caregiver/s. This may cause them to fully wake and signal at the end of every sleep cycle, rather than just stirring and falling back into the next sleep cycle.
Separation stress may be a likely cause of frequent waking if you find your little one sleeps soundly for decent stretches when close to you / when they can sense your presence, but is very wakeful when they sleep in their own bed/room.
Having them sleep close to you – either in their own bed within arm’s reach, or safely bedsharing (you can find the safe co-sleeping guidelines here) if that’s an option available to you, can help with this.
4) Other stressful events/periods
A stressful event or period in your little one’s life can also affect sleep.
This is because when the body’s stress response system (the HPA-axis / sympathetic nervous system) is activated, it can make it hard to fall asleep / stay asleep. Little ones experiencing stress may also have a heightened need to be close to their parent/caregiver when they sleep.
Common possiblities include starting daycare, adjusting to a change in caregivers, the arrival of a new sibling, and other big changes / events (including family gatherings, travel etc.).
Some little ones will not find these changes particularly stressful while others may, so it does depend on the individual, but certainly something to keep in mind if you’ve noticed an increase in night wakefulness that coincides with a stressful event or period.
If you’re pretty sure this is the cause of the wakefulness, then it will usually be a case of riding it out and supporting your little one as best you can by responding to / meeting their needs (which may include having them sleep close to you/another trusted caregiver at night), and working with any other caregivers to do the same.
5) Lower than optimal sleep pressure
This is not commonly focused on out there in the world of baby sleep (yet!) but has to be the most common cause of frequent night waking that I see!
Sleep pressure – officially referred to as sleep/wake homeostasis – is one of the two systems in our body that regulates sleep. It’s actually a chemical called adenosine that builds up in our brain while we’re awake, and reduces while we sleep. The higher our sleep pressure (adenosine levels), the sleepier we feel and the more we need to sleep to reduce it down again.
For a ‘solid’ night’s sleep (one where we sleep relatively soundly, for decent stretches), sleep pressure needs to build to a high enough level by bedtime.
If it doesn’t, then we can have trouble falling asleep, or become wakeful at some stage during the night, or wake really early the next morning (or a combination of these!).
Babies – being humans – are not really much different to adults in this way.
If they’re not tired enough when they go to bed, they may resist sleep / take a long time to fall asleep, or they may sleep lightly and struggle to link sleep cycles for part or all of the night.
You might find they have ‘false starts’ (frequent waking in the first hour or two after first going to bed), or they might sleep quite well in the first part of the night and then wake frequently in the second half, or, they may just wake hourly or more often for the whole night.
Regardless of what the wakefulness looks like, if low sleep pressure is the culprit, the good news is that it is usually possible to improve the nights, without any form of sleep training.
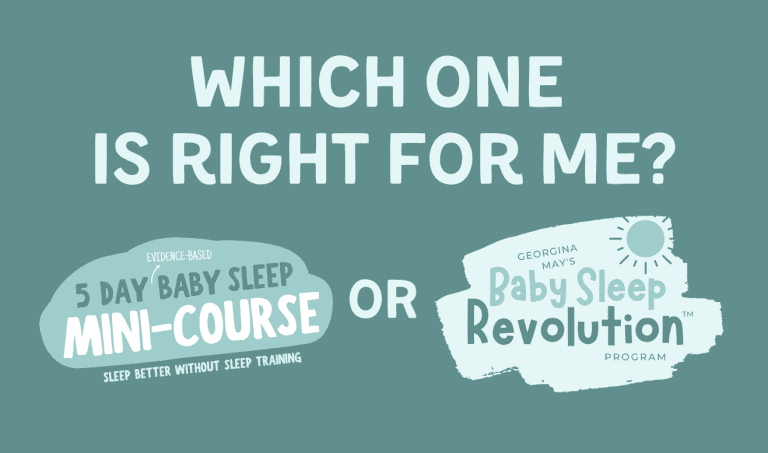
It’s what I help parents with every day in my 5 Day Baby Sleep Mini-Course and my unique, flagship program – Baby Sleep Revolution™.
So if you’re struggling with frequent night waking, and you’ve ruled out the other likely causes, definitely have a look at both options!
For most parents, the 5 Day Baby Sleep Mini-Course is the best place to start (and may be all you need) because often you can improve sleep with just a few tweaks and changes, but if you’re struggling to function and need to improve the nights ASAP, or you’re already familiar with sleep pressure / have already tried a solution or approach aimed at increasing sleep pressure, then you may want to jump straight to the Baby Sleep Revolution™ program.
If you’re unsure which one is right for you – I’ve got a short video and blog post that explains the differences between the two here.
Georgina x
References:
[1] Kahn, A., Rebuffat, E., Blum, D., Casimir, G., Duchateau, J., Mozin, M. J., & Jost, R. (1987). Difficulty in initiating and maintaining sleep associated with cow’s milk allergy in infants. Sleep, 10(2), 116–121. https://doi.org/10.1093/sleep/10.2.116
[2] Ramirez, F. D., Chen, S., Langan, S. M., Prather, A. A., McCulloch, C. E., Kidd, S. A., Cabana, M. D., Chren, M. M., & Abuabara, K. (2019). Association of Atopic Dermatitis With Sleep Quality in Children. JAMA pediatrics, 173(5), e190025. https://doi.org/10.1001/jamapediatrics.2019.0025
[3] Edmunds, J., Miles, S. C., & Fulbrook, P. (2011). Tongue-tie and breastfeeding: a review of the literature. Breastfeeding review : professional publication of the Nursing Mothers’ Association of Australia, 19(1), 19–26. https://pubmed.ncbi.nlm.nih.gov/21608523/
[4] Peirano, P. D., Algarín, C. R., Chamorro, R. A., Reyes, S. C., Durán, S. A., Garrido, M. I., & Lozoff, B. (2010). Sleep alterations and iron deficiency anemia in infancy. Sleep medicine, 11(7), 637–642. https://doi.org/10.1016/j.sleep.2010.03.014
[5] Czinn, S. J., & Blanchard, S. (2013). Gastroesophageal reflux disease in neonates and infants : when and how to treat. Paediatric drugs, 15(1), 19–27. https://doi.org/10.1007/s40272-012-0004-2
[6] Richdale, A. L., & Schreck, K. A. (2009). Sleep problems in autism spectrum disorders: prevalence, nature, & possible biopsychosocial aetiologies. Sleep medicine reviews, 13(6), 403–411. https://doi.org/10.1016/j.smrv.2009.02.003
[7] Cohen, S., Conduit, R., Lockley, S. W., Rajaratnam, S. M., & Cornish, K. M. (2014). The relationship between sleep and behavior in autism spectrum disorder (ASD): a review. Journal of neurodevelopmental disorders, 6(1), 44. https://doi.org/10.1186/1866-1955-6-44
[8] Owens J. A. (2009). A clinical overview of sleep and attention-deficit/hyperactivity disorder in children and adolescents. Journal of the Canadian Academy of Child and Adolescent Psychiatry = Journal de l’Academie canadienne de psychiatrie de l’enfant et de l’adolescent, 18(2), 92–102. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2687494/